Growing
stronger
every day
THE WORLD’S PREMIERE &
LARGEST FAITH-BASED
MENTAL HEALTH ORGANIZATION
CARE AND COUNSEL TOOLS
Featured Resources & Services
Join us at our live events
DSM-5-TR – What Mental Health Professionals Need to Know
Quick Guide to the DSM-5-TR – What Mental Health Professionals Need to Know Recently, the American Psychiatric Association released the DSM-5-TR, which includes a fully revised text and references, updated diagnostic criteria, and ICD–10–CM codes. The DSM–5 was previously published in 2013. Below, you will find a compiled list of changes with downloadable fact sheets provided by the American Psychiatric […]
AACC BLOG
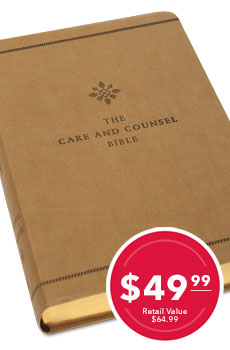
2024 Monthly Counseltalk Webinars
Web based training resources provided by the American Association of Christian Counseling. We offer two live webinars every month which can be used for continuing education credit. These webinars are free for our AACC Presidential Members but can be purchased separately for non members as well.
Sign Up for a
Free Webinar!
AACC Counseltalk Webinars are presentations on a variety of topics transmitted over the Web to those in the helping profession. Webinar participants receive valuable insight from professionals in their respective fields from the comfort of their homes or offices and can earn continuing education hours (CE’s) required for maintaining specialized mental health licensures and certifications.

MISSION OF THE AACC
AACC is committed to assisting Christian counselors, the entire “community of care,” licensed professionals, pastors, and lay church members with little or no formal training.
It is our intention to equip clinical, pastoral, and lay care-givers with biblical truth and psychosocial insights that minister to hurting persons and help them move to personal wholeness, interpersonal competence, mental stability, and spiritual maturity.
Platinum Elite Partners

Platinum Partners